Radiotherapy can treat all solid tumours, however the dose is limited by toxicity to the surrounding healthy tissue. It is well established that small increases in x-ray dose gives significant improvements in treatment outcomes. Our product Oxilia substantially increases the dose of radiotherapy without damaging healthy tissue.
Radiotherapy
Oxilia injection
Higher cure rates
Fewer side effects
More treatable cancers
Oxilia Nanoparticles
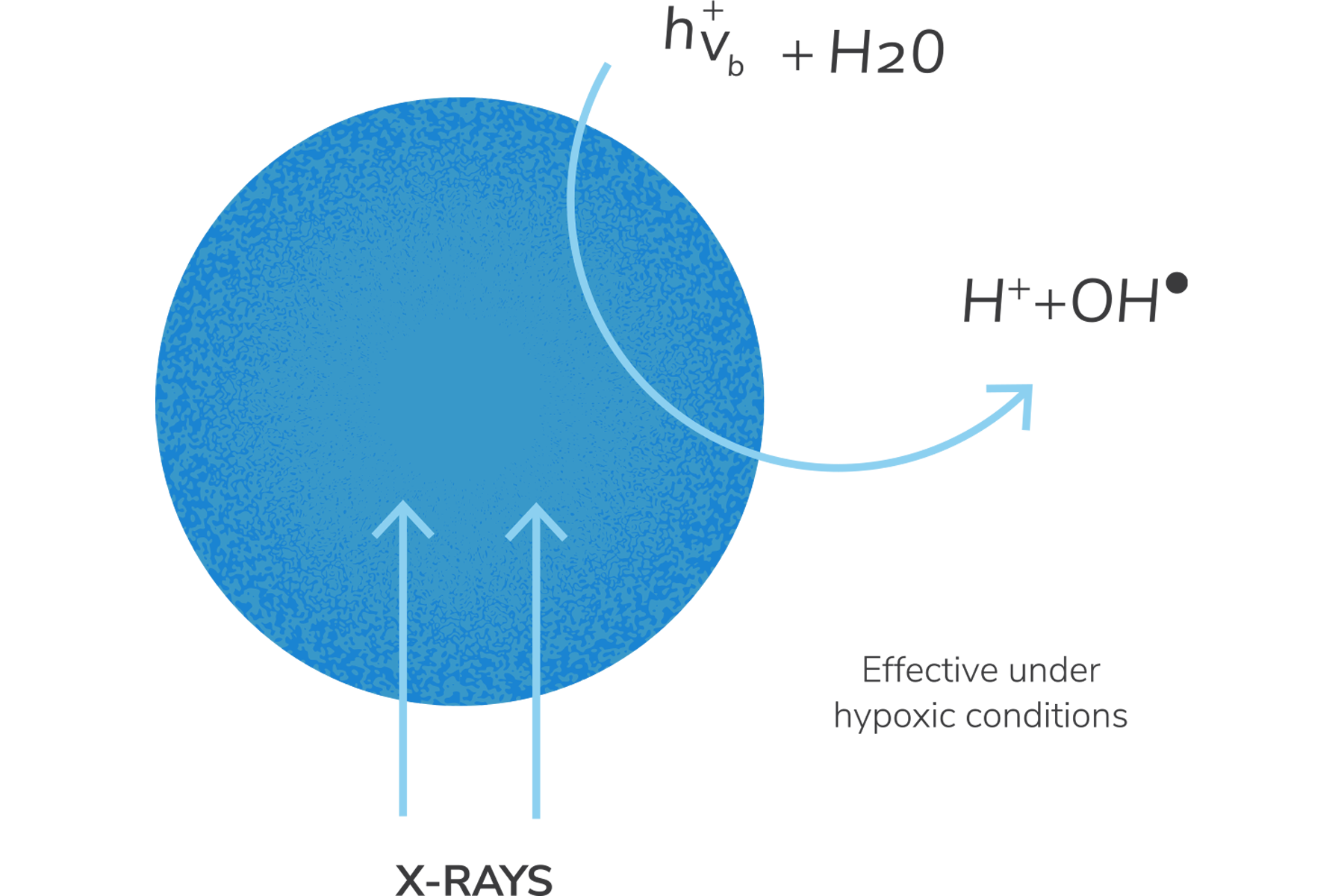
Oxilia nanoparticles are based on the photoactive properties of titanium dioxide and the ability of rare earth elements to absorb ionizing radiation.
Key Features |
|
|---|---|
| 50nm particle size | Optimal size for cancer cell uptake |
| Particle doped with rare earths | Strongly absorb X-rays |
| Highly photoactive TiO2 particle | Free radicals generated from particle surface |
| TiO2 generates free radicals by splitting water | Effective in hypoxic tumours otherwise resistant to radiotherapy |
| TiO2 completely inert in body | Non toxic, widely used food additive (E171) |
Delivering unparalleled dose enhancement
Oxilia nanoparticles are injected into tumours in a single low volume procedure prior to radiotherapy. The inert nanoparticles accumulate in cancer cells and absorb ionizing radiotherapy to split water and generate cancer killing free radicles even in hypoxic tumours. In this way Oxilia enhances the effect of radiotherapy which is otherwise dependent on the presence of oxygen.
Oxilia is only active when the beam is switched on – it is completely inert outside of treatment.
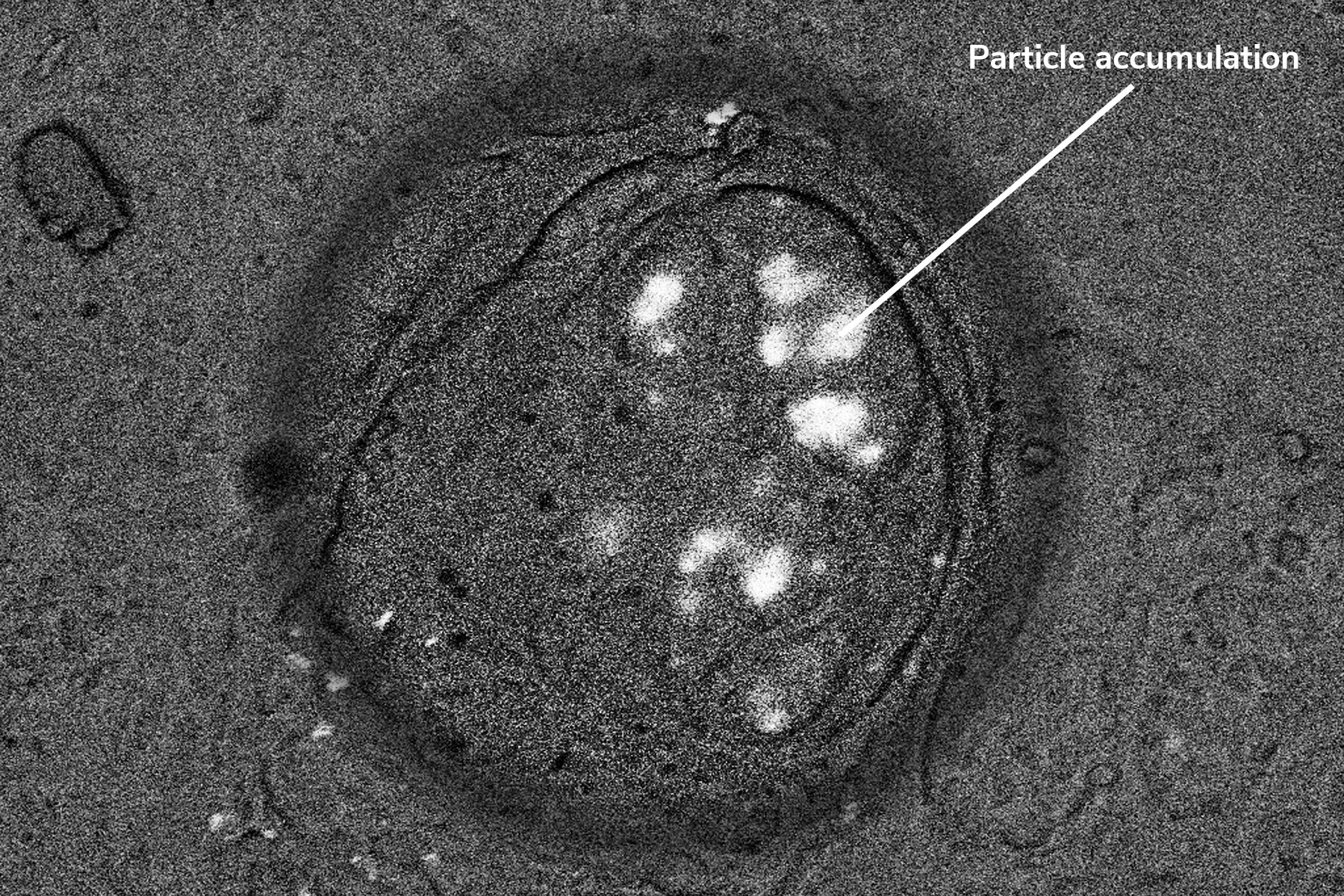
Particles accumulate in cancer cells
Oxilia particles accumulate in cancer cells and are retained throughout the period of radiotherapy. (fig 1.)
fig 1.
In Vivo Efficacy in Multiple Solid Tumours
Mouse xenograft – Colo205 colorectal carcinoma (Balb/c nude mice)
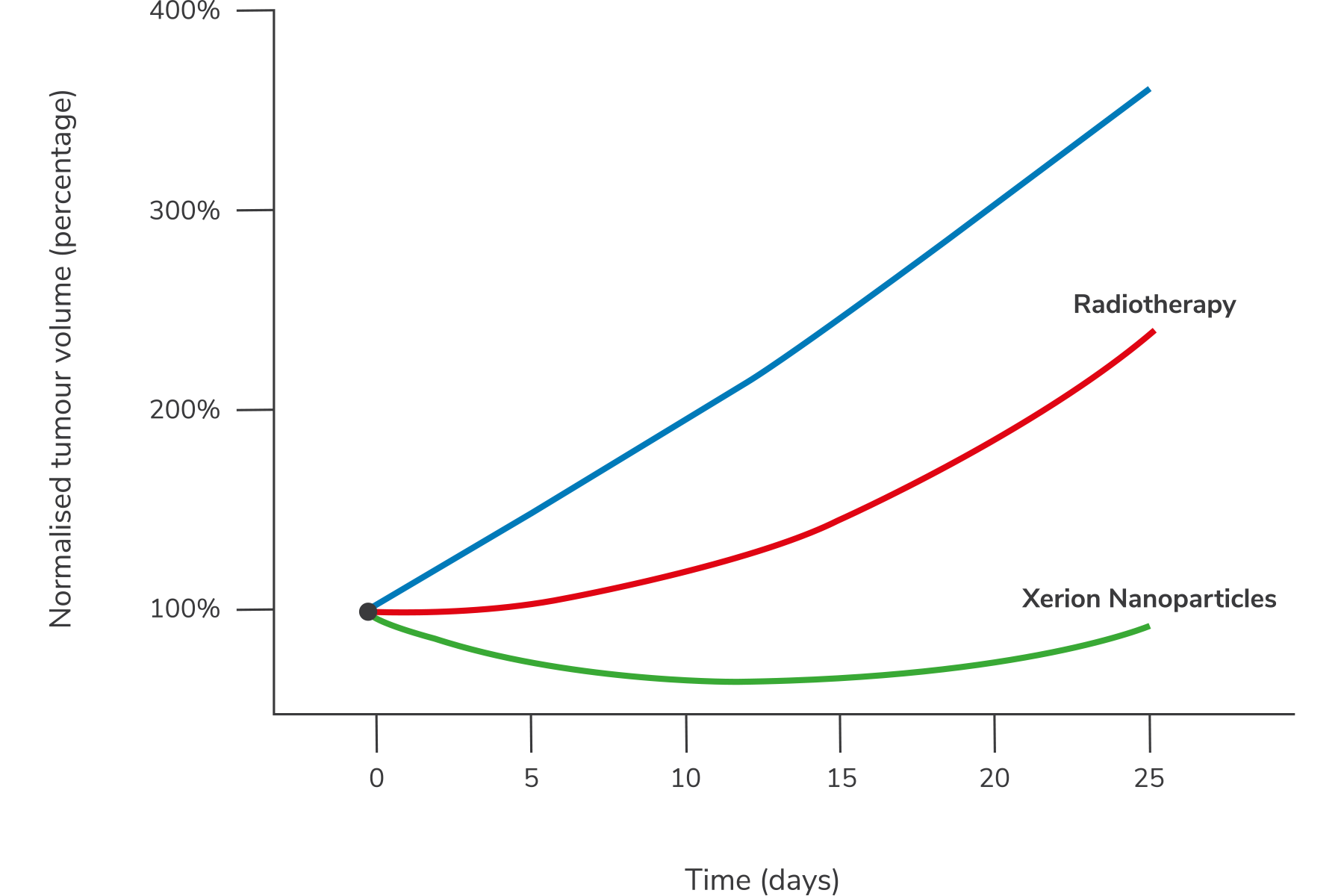
— Control
— 10Gy radiotherapy
— 10Gy radiotherapy plus nanoparticles
Study by Crown Bioscience (San Diego)
Potential tumour targets
Oxilia has a generic, physical mode of action that can target a wide range of poorly treated solid tumours. Xerion’s initial focus is on head and neck cancer.
Head and neck cancers
Head and neck cancers are tumours of the epithelial cells from the lip to the top of the oesophagus. Survival rates vary greatly by site – from 96% survival with lip cancers to less than 20% survival from hypopharyngeal tumours deep in the throat. Just over 40% of head and neck cancers are tumours of throat which are often impossible to remove surgically.
Best supported care
- 70Gy radiotherapy (35 x 2Gy) with concurrent cisplatin
- Cisplatin poorly tolerated with serious side effects
- Many patients too weak to receive cisplatin
Over 40% of head and neck cancers are tumours of the throat which are often impossible to remove surgically.
Pancreatic cancer
Pancreatic cancer has the worst prognosis of all common cancers, having 1 and 5 year survival rates of 12% and 3% respectively. Survival rates have not improved over the last forty years, indicating a critical need for innovative treatments for this devastating disease. Tumours are often diagnosed at advanced stage, surgery is impossible for 96% of patients, chemotherapy has little effect and radiotherapy is used in palliative mode only.
Pancreatic tumours are often diagnosed at advanced stage, surgery is impossible for 96% of patients.
Improvement over radiotherapy alone
Human cancer in mouse model, assessed by time to double tumour volume.
Oropharyngeal
(FaDu)
1.7x
Pancreatic
(MIAPaCa)
2.5x
Oropharyngeal
(Colo205)
2.7x

